Digestive problems are often an embarrassment, and many people understandably try to hide their issues. It’s important to know, however, that you are certainly not alone.
The most common digestive symptoms include:
- I have Gas- to mean bloating, belching, fullness
- Difficulty in swallowing
- Nausea and vomiting
- Change of Appetite- Poor or excessive appetite
- Vomiting of blood
- Bleeding per rectum or black coloured stools
- Unintentional weight loss
- Diarrhoea
- Constipation
- Jaundice
- Abdominal pain or cramps
- Swollen legs with general weakness
The symptom of I have ‘Gas’!
Patients commonly complain of “gas” a condition they like to describe a group of symptoms rather than one predominant symptom.
These symptoms include:Belly discomfort, bloating, feeling uncomfortably full after eating, nausea, heart burn, burping of food or liquids, loss of appetite.
These symptoms are collectively called ‘Dyspepsia’ in medical parlance.
What causes dyspepsia?
The common causes of dyspepsia include:
Burped-up stomach juices and regurgitation or reflux caused by gastroesophageal reflux disease (GERD) or a hiatal hernia (Ref: GERD).
Lactose intolerance: An inability to digest milk and dairy products
Cholecystitis: Gallbladder pain (biliary colic) or inflammation due to stones.
Medicines: Examples of medicines that may cause dyspepsia are aspirin and similar drugs, antibiotics, steroids, digoxin, and theophylline. Peptic (stomach) ulcer or duodenal ulcer
Anxiety or depression due to various domestic or work related causes.
Alcohol and caffeine (in coffee or tea)
Even stomach cancer can present with such symptoms.
How can I have relief of dyspepsia?
You should be willing to make changes to your lifestyle to help relieve your symptoms of dyspepsia. Here are some suggestions to try:
- Lose weight if you need to. Losing just 5 to 10 pounds can help.
- Change your eating habits.
It’s best to eat several small meals instead of two or three large meals. After you eat, wait 2 to 3 hours before you lie down. Late-night snacks aren’t a good idea.
Chocolate, mint, and alcohol can make dyspepsia worse. They relax the valve between the food pipe and the stomach.
- Avoid Spicy foods, foods that have a lot of acid (like tomatoes and oranges), and coffee can make dyspepsia worse in some people. If your symptoms are worse after you eat a certain food, you may want to stop eating that food to see if your symptoms get better.
- Do not smoke or chew tobacco.
If you get dyspepsia at night, raise the head end of your bed 6 to 8 inches by putting a bolster under the head of your mattress. Do not wear tight clothing around your middle.
Difficulty in swallowing
What is difficulty in swallowing (dysphagia)?
Difficulty swallowing is also called dysphagia. It is usually a sign of a problem with your throat or food pipe-the muscular tube that moves food and liquids from the back of your mouth to your stomach. Although dysphagia can happen to anyone.
Some of these are minor, and others are more serious. If you have trouble swallowing on a regular basis, you may have a more serious problem that needs treatment.
What causes dysphagia?
Normally, the muscles in your throat and esophagus squeeze, or contract, to move food and liquids from your mouth to your stomach without problems. Sometimes, though, food and liquids have trouble getting to your stomach. There are two types of problems that can make it hard for food and liquids to travel down your esophagus:
The muscles and nerves that help move food through the throat and esophagus are not working right. This can happen if you have:
- Gastroesophageal reflux disease (GERD): When stomach acid backs up regularly into your esophagus. it can cause ulcers in the esophagus, which can then cause scars to form. These scars can make your esophagus narrower.
- Esophagitis: This is inflammation of the esophagus. This can be caused by different problems, such as GERD
- Esophageal tumors. Growths in the esophagus may be cancerous or non cancerous.
- Esophageal spasm: This means that the muscles of the esophagus suddenly squeeze. (Eg.,Achalasia)
What is achalasia?
Achalasia is a rare disorder of the oesophagus. It is characterized by enlargement of the oesophagus, impaired ability to push food down toward the stomach (peristalsis), and failure of the muscle at the lower part of the esophagus, the lower esophageal sphincter (LES), to relax. It is the contraction and relaxation of the sphincter that moves food through the tube.
What is the treatment for Achalasia?
Treatment options and recommendations are as follows:
- Initial therapy choice should be based on patient age, sex, preference, and local institutional expertise
- Pharmacologic therapy consisting of of nitrates and calcium channel blockers are most commonly used for patients
- Graded pneumatic dilation (PD) is considered in some cases
- Surgical myotomy by Per Oesophageal Endoscopic Myotomy ( POEM) is the latest procedure where the offending constriction is divided by endoscopy. Earlier the same was accomplished laparoscopically.
- Botulinum toxin therapy is recommended for patients not suited to PD or surgery.
Nausea and vomiting
Nausea is an uneasiness of the stomach that often comes before vomiting. Vomiting is the forcible voluntary or involuntary emptying (“throwing up”) of stomach contents through the mouth.
What Causes Nausea or Vomiting?
The causes of vomiting differ according to age. For children, it is common for vomiting to occur from a viral infection, food poisoning, milk allergy, motion sickness, overeating or feeding, coughing, or blocked intestines and illnesses in which the child has a high fever.
Nausea and vomiting are not diseases, but they are symptoms of many conditions such as:
Motion sickness or seasickness, excessive amounts of alcohol, medication-induced vomiting, intense pain due to stones in the kidney or gallbladder, early stages of pregnancy, Emotional stress, food poisoning, overeating, Heart attack, concussion or brain injury, brain tumour, peptic ulcers, complication of uncontrolled diabetes,
What are the remedies for Nausea and Vomiting of short duration?
The timing of the nausea or vomiting can indicate the cause. When appearing shortly after a meal, nausea or vomiting may be caused by food poisoning, gastritis (inflammation of the stomach lining) or an ulcer. Nausea or vomiting one to eight hours after a meal may indicate food poisoning. A careful and insightful history into the recent intake may give a clue. Treatment varies according to the cause. Usually responds to anti emetics and fluid therapy supplemented with specific treatment addressed toward the cause.
Is Vomiting Harmful?
Usually, vomiting is harmless, but if prolonged it can be a sign of a more serious illness. Some examples of serious conditions that may result in nausea or vomiting include concussions, meningitis., intestinal blockage and brain tumors.
Recurrent vomiting can cause dehydration. Young children have a greater risk of becoming dehydrated compared to adults.
How Is Vomiting Treated?
Avoid solid food until the vomiting episode has passed
If vomiting and diarrhea last more than 24 hours, an oral rehydrating solution should be used to prevent and treat dehydration.
Vomiting associated with cancer treatments can often be treated with another type of drug therapy.
There are drugs that can be used to control vomiting associated with motion sickness. However, consult with a doctor before using any of these treatments.
How Can I Prevent Nausea?
- Eat small meals throughout the day instead of three large meals.
- Eat slowly, avoid hard-to-digest foods.
- Drink liquids between meals rather than during meals.
- Try to eat when you feel less nauseated.
If the vomiting has been present for long what shall I do?
Symptom of vomiting often for days on may be indicative of an underlying disease as explained above. Requires suitable investigations to identify the cause since there are many conditions and diseases which can cause prolonged vomiting. You must visit your doctor for guidance and treatment.
Appetite changes- decreased and increased appetite
Common Causes
Some of the common causes of loss of Appetite may include:
- Alcoholism
- Gastritis
- Peptic ulcer
- Drug related
- Malabsorption
- Hypothyroidism
- Hiatus hernia
- Chemotherapy
- Heart failure
- Anxiety and depression etc.
Some of the common causes of increased Appetite may include:
- Anxiety.
- Certain drugs (NSAIDS, corticosteroids etc.)
- Bulimia (most common in women 18 – 30 years old)
- Diabetes mellitus
- Graves’ disease ( Hyperthyroidism).
- Hypoglycemia.
- Premenstrual syndrome.
When to Contact a Medical Professional?
Contact your doctor if:
- You have an unexplained, persistent increase in appetite
- You have other unexplained symptoms.
Bleeding from GI tract- Vomiting of blood
A variety of conditions can cause bleeding in the upper digestive tract. Locating the source of bleeding is an important step to help the doctor find the cause of the bleeding. Different conditions can cause bleeding in the upper GI tract.
The causes of bleeding per rectum are described separately.
Causes of bleeding in the upper GI tract may include
- Peptic ulcers—sores in the lining of the oesophagus, stomach, or duodenum. The bacteria Helicobacter pylori (H. pylori) and use of pain killers- aspirin or the nonsteroidal anti-inflammatory drugs (NSAIDs) can cause peptic ulcers.
- Oesophageal varices—enlarged blood vessels in the oesophagus (food pipe) that can leak blood or even rupture, causing life-threatening bleeding. Oesophageal varices are usually associated with a chronic liver condition called cirrhosis.
- Mallory-Weiss tear— Severe vomiting causes tears in the lower end of the oesophagus ( food pipe)
- Gastritis—a condition in which the stomach lining is inflamed. Some common causes of gastritis include the use of aspirin, NSAIDs and other medications, infections, critical illnesses, and severe injuries. If untreated, gastritis can lead to ulcers or erosions in the stomach lining that can bleed.
What are the signs and symptoms of bleeding in the digestive tract?
The signs and symptoms of bleeding in the digestive tract depend on the location and severity of bleeding.
Signs and symptoms of bleeding in the upper or lower GI tract may include
- acute bleeding, which may include abdominal cramps
- bright red blood in vomit
- dark or bright red blood mixed with stool
- vomit that looks like coffee grounds
- black or tarry stool
- dizziness or faintness
- shortness of breath
Chronic bleeding.
A person with chronic bleeding may develop anaemia, a condition in which red blood cells are fewer than normal, which prevents the body’s cells from getting enough oxygen. Symptoms of anaemia may include fatigue and shortness of breath, which can develop over time.
Some people may have occult bleeding. Occult bleeding may be a sign of inflammation or a disease such as colorectal cancer. A simple lab test can detect occult blood in the stool.
Bleeding per rectum or black coloured stools
What are the causes of bleeding in the lower GI tract ?
- Haemorrhoids (piles). Hemorrhoids are swollen and inflamed veins around the anus or in the lower rectum. Constipation and straining during bowel movements cause the veins to swell. Hemorrhoids cause itching, pain, and sometimes bleeding.
- Fissures are small tears in the anus that can cause bleeding.
- Colitis — inflammation of the colon. A complication of colitis is ulcers in the large intestine eg., ulcerative colitis that can cause bleeding.
- Colon polyps — abnormal growths of tissue in the lining of the colon and rectum can cause bleeding.Some types of polyps may already be cancerous or can become cancerous.
- Angiodysplasia — abnormal or enlarged blood vessels in the lower GI tract that can become fragile and bleed.
How is the cause of bleeding in the digestive tract diagnosed?
To diagnose bleeding in the digestive tract, your doctor will first determine the site of the bleeding based upon the following:
- medical and family history
- physical exam
- lab tests
- nasogastric lavage
- upper GI endoscopy, enteroscopy, and capsule endoscopy
- colonoscopy or flexible sigmoidoscopy
- imaging tests
The Imaging Tests
To help find the cause of digestive tract bleeding, your doctor may order one or more of the following imaging tests.
- Abdominal computerized tomography (CT) scan.Angiogram. An angiogram is a special kind of x ray in which an interventional radiologist threads a thin, flexible tube called a catheter through the large arteries, often from the groin, and injects contrast medium through the catheter so the artery and site of bleeding show up more clearly on the x ray..Radionuclides scan. A radionuclides scan can help find the cause of digestive tract bleeding.
How is bleeding in the digestive tract treated?
Treatment depends on the cause or location of the bleeding. During a colonoscopy, or an endoscopy, a gastroenterologist can stop the bleeding by endoscope or colonoscope to
- inject medications into the bleeding site
- treat the bleeding site and surrounding tissue with a heat probe, an electric current, or a laser
- close the affected blood vessels with a band or clip
An interventional radiologist can use an angiogram to inject medications or other materials into blood vessels to stop some types of bleeding.
When infections or ulcers cause the bleeding, medications are prescribed to treat the problem.
When a person has severe acute bleeding or bleeding that does not stop by all means, a surgeon may need to perform a laparotomy( opening of abdomen) to stop the bleeding.
How can bleeding in the digestive tract be prevented?
People can prevent some of the causes of digestive tract bleeding by
- limiting the amount of NSAIDs they take
- following doctors advise for treatment of cirrhosis liver
Eating, Diet, and Nutrition
People can prevent digestive tract bleeding by avoiding spicy foods, alcoholic drinks and smoking, that can increase stomach acids and lead to ulcers.
People who have a history of diverticular disease, anal fissures, and hemorrhoids should follow the diet their health care provider recommends to help prevent repeat bleeding.
Unintentional weight loss
Unintentional weight loss is when you lose weight without dieting or increasing physical activity. It may occur following a loss of appetite or when you’re consuming the same amount of calories as usual. Either way, it’s usually a cause for concern.
Unintentional weight loss can be extremely distressing, particularly when you lose a relatively significant amount and don’t know why. Unintentional weight loss could be a sign of serious illness or disease, or it could be something as minor as a stomach virus.
Unintentional weight loss is often the result of a variety of diseases like malnutrition, diabetes, hyperthyroidism (overactive thyroid gland), abdominal infection, gastroenteritis, cancer, celiac disease, and HIV or AIDS.
Long periods of weight loss can lead to malnutrition. Malnutrition occurs when you aren’t consuming a proper amount of nutrients. This can be especially true for those with a digestive disorder such as celiac disease, which affects how the body absorbs nutrients.
How Is Unintentional Weight Loss Diagnosed?
Your doctor must go over your symptoms and any recent lifestyle changes you’ve made to know exactly what’s causing the weight loss.
Your doctor may ask the following questions: Have you changed your diet? Have you had a recent illness? Have you recently traveled out of the country? Are you less energetic than usual? Have you had any digestive problems, such as diarrhea or constipation? Have you started taking any new medications?
Investigations
If your doctor feels that your diet or a digestive disorder is to blame, blood tests to assess levels of specific vitamins and minerals including serum iron levels related may be ordered. Blood tests can also determine if a hormonal condition is to blame. A chest X-ray to rule out tuberculosis is considered. Endoscopic evaluation of your stomach and large bowel may be ordered. Biopsy of duodenum may be done to identify the status of villi.
Sometimes if the results do not point to any specific cause, capsule endoscopy will be considered to study the small bowel for identifying the cause.
What Are the Treatment Options for Unintentional Weight Loss?
If you have a nutritional deficiency, your doctor may refer you to a dietitian to devise a diet plan that helps to correct the deficiency.
A deficiency due to a digestive disorder, such as inflammatory bowel disease, may require a specialized diet during times of inflammation to help you get the nutrients you need. This may include taking over-the-counter supplements.
Your doctor will likely prescribe medication if a hormonal disorder is causing the unintentional weight loss.
You can correct unintentional weight loss due to tuberculosis, diabetes.
If your doctor suspects that your unintentional weight loss may be due to a more serious illness, such as cancer, you may undergo some tests to get more information.
DIARRHOEA
What Is Diarrhoea?
Diarrhoea is watery loose stools that occur urgently and frequently at least three times a day. It’s also often associated with belly pain, cramping, nausea, gas, and bloating.
Diarrhoea that only lasts a few days is called acute diarrhoea. Chronic diarrhoea, on the other hand, can last for weeks or even months, leading to serious health complications.
What causes diarrhoea?
Many things can trigger diarrhoea, including viral, bacterial, or parasitic infection
adverse reaction to medication, intestinal disorders such as Tuberculosis, Malabsorption, celiac disease, irritable bowel syndrome (IBS), allergy or intolerance to food (like dairy products)and inflammatory bowel diseases like ulcerative colitis and Crohn’s disease.
What Can I Do About Diarrhoea?
If you experience a bout of diarrhoea, you should:
Drink plenty of fluids (including water, broth, fruit juices, and sports drinks)
Avoid dairy products and fatty foods,
Stick to mild foods that won’t aggravate your stomach, like idlis, dry toast, clear broth soups, and rice..
When should diarrhoea be Treated?
Generally, acute cases of diarrhoea will clear up without treatment. But, it’s important to drink lots of fluids because even brief cases of diarrhoea can lead to profound dehydration.
People with chronic diarrhoea are also at risk of malnutrition because the body becomes unable to absorb foods properly.
When should I consult a doctor?
If your diarrhoea is accompanied by intense abdominal pain, fever, or dehydration, contact your doctor.
Chronic diarrhoea, which persists for longer than two weeks, should be evaluated and treated by a doctor. It may be due to irritable bowel syndrome, tuberculosis of intestines, chronic non specific infections, or mal absorption. After testing your stool for bacteria, viruses, and parasites, your doctor may prescribe medicines.
What if I have chronic diarrhoea?
You may need to undergo blood investigations including some specific tests to identify the cause, colonoscopy & biopsy, capsule endoscopy etc.
How is diarrhoea in children different from adults?
Diarrhoea can be particularly serious in children, since they tend to become dehydrated more quickly than adults. Don’t hesitate to call your pediatrician if your child experiences persistent diarrhea
Constipation
Constipation occurs when you have fewer than three bowel movements in a week. Constipation is a common digestive issue in which bowel movements are infrequent or difficult to pass. It’s considered a symptom of various health issues, rather than a disease by itself.
What is normal bowel habit?
“Normal” bowel habits differ between people. Some people may pass stool three times a day, while others may only have a bowel movement three times a week.
Is it normal if I have bowel movement only on alternate days?
You’re considered constipated if you have fewer than three bowel movements in a week. After this point, your stool may harden and become difficult or even painful to pass.
What are the risks of constipation?
Constipation is one of the most common gastrointestinal (GI) issues.
- Hemorrhoids (piles)
- Anal fissures (small tears in the anus accompanied by pain and bleeding)
- Fecal impaction
- Rectal prolapse (a part of the rectum sticks out of the anus)
What causes constipation?
- Lack of fiber in the diet
- Lack of physical activity and low fluid intake
- Certain medications (such as antidepressants, painkillers, antacids and iron supplements
- Poor bowel habits (ignoring the urge to go)
- GI tract disorders such as irritable bowel syndrome, tumors or colon polyps
- Diseases including like diabetes, hypothyroidism, Parkinson’s disease, stroke
How do I prevent constipation?
- By getting the right amount of fibre through eating more fruits, leafy vegetables, and whole-grain cereals
- Regularly drinking water and other healthy beverages
- Exercising regularly
- Trying to have a bowel movement at the same time every day, such as 15 to 45 minutes after breakfast (eating stimulates colon activity)
- Not resisting the urge to have a bowel movement
What if the above measures fail?
If dietary and lifestyle changes alone are unable to fully relieve constipation, laxatives may help. But you shouldn’t take any constipation medications before discussing with your doctor.
Medications include bulk-forming and osmotic laxatives, stool softeners, lubricants, and if your constipation is severe stimulant laxatives may help.
Does constipation require investigations?
Chronic constipation requires systematic investigation to exclude the presence of any underlying endocrinal disorders (like diabetes and hypothyroidism), obstruction of large intestine due to tumours or presence of any anatomical abnormalities. For this your doctor may order blood investigations, colonoscopy and ano-rectal manometry to study the functional integrity of your ano-rectal system
What is bio feed back mechanism?
Chronic constipation is sometimes caused by a dysfunction of the anorectal muscles. Your doctor may recommend biofeedback, a procedure that involves monitoring muscle activity with special sensors, to retrain your muscles to work properly.
All you want to know about jaundice
What is Jaundice?
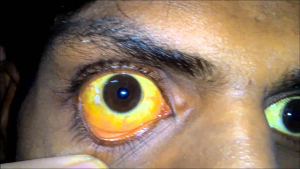
 Jaundice occurs when the skin, sclera (whites of the eyes) and mucous membranes of oral cavity turn yellow.
Jaundice occurs when the skin, sclera (whites of the eyes) and mucous membranes of oral cavity turn yellow.
This yellow color is due to a high level of bilirubin, a yellow-orange bile pigment. Bile is a fluid secreted by the liver. Bilirubin is formed from breakdown of red blood cells. The normal bilirubin level in blood plasma is below 1.2 mg/dL (≶25µmol/L). A concentration higher than approx. 3 mg/dL (>50µmol/L) leads to jaundice.
How true is that there is no treatment for jaundice in modern medicine (some choose to call Allopathy).
 It is not at all true. Most commonly seen jaundice is caused by Hepatitis A virus which is a self limiting disease. Except for supportive measures, it doesn’t really require any anti viral treatment. And this scientific approach to disease has been erroneously taken by the public as no availability of treatment.
It is not at all true. Most commonly seen jaundice is caused by Hepatitis A virus which is a self limiting disease. Except for supportive measures, it doesn’t really require any anti viral treatment. And this scientific approach to disease has been erroneously taken by the public as no availability of treatment.
Only the modern medicine has comprehensive treatment protocols for various types of jaundice including surgery, which may be needed sometimes to correct the jaundice.
But why the public in general think grandma home remedies are best for jaundice and modern medicine is a big no no?
 A self limiting jaundice of the kind explained above clears off on its own. But some unduly take credit if the jaundice subsides on administering herbal medicines. Sometimes such medicines can be toxic to the already damaged liver. There are different types of jaundice due to various causes (refer below) and the treatment is not same for all. Herbal medicines cannot give relief for all types of jaundice.
A self limiting jaundice of the kind explained above clears off on its own. But some unduly take credit if the jaundice subsides on administering herbal medicines. Sometimes such medicines can be toxic to the already damaged liver. There are different types of jaundice due to various causes (refer below) and the treatment is not same for all. Herbal medicines cannot give relief for all types of jaundice.
Why do people indulge in self medication?
Most people have a false notion that all that is naturally available costs much less, harmless and free of ill effects. They do not realize that it is not necessarily true that all natural products are effective and harmless.
Under a false hope of easy cure, most people resort to self medication unaware of the dangers of toxic effects of native medicines supplied by unqualified people. They keep postponing investigations to identify the true nature of jaundice. This undue delay some times proves very costly not only to the patient but also the entire family in monetary terms when the disease reaches incurable stage. At times it can cost the life.
What will happen if a person indulges in self medication and refuses to go to a doctor?
 Jaundice may be the presenting feature of certain cancers and deadly viruses. Self medication can delay investigation of the cause. This delay in seeking proper professional advice can make an otherwise curable viral disease or cancer incurable. The right approach is to seek and follow professional advice.
Jaundice may be the presenting feature of certain cancers and deadly viruses. Self medication can delay investigation of the cause. This delay in seeking proper professional advice can make an otherwise curable viral disease or cancer incurable. The right approach is to seek and follow professional advice.
What will the doctor do when I consult with jaundice?
At first the doctor examines you and assesses your health condition and orders relevant blood tests including Liver Function Tests (LFT) and an ultrasound scan. Blood tests will estimate the level of bilirubin to gauze the severity of jaundice. The liver enzymes and other liver tests give an idea of the status of liver function.
Ultrasound Scan (USG) study can identify stones in the gallbladder and the bile duct which can obstruct the out flow of bile from liver and cause jaundice. If USG study is unclear, MRI scan is ordered to identify cancer related blockages of the bile duct, the cause of jaundice and this is one of the most useful methods of establishing a provisional diagnosis .
What are the symptoms of jaundice?
 The severity of symptoms depends on the underlying causes and how quickly or slowly the disease progresses. Sometimes, there may not be symptoms and the condition may be found accidentally. If you have a short-term case of jaundice (usually caused by infection) you may have the following symptoms:
The severity of symptoms depends on the underlying causes and how quickly or slowly the disease progresses. Sometimes, there may not be symptoms and the condition may be found accidentally. If you have a short-term case of jaundice (usually caused by infection) you may have the following symptoms:
- Fever
- Chills
- Abdominal pain
- Flu-like symptoms
- Change in skin color
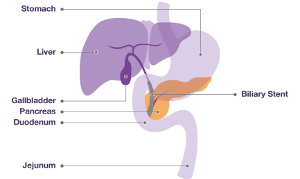
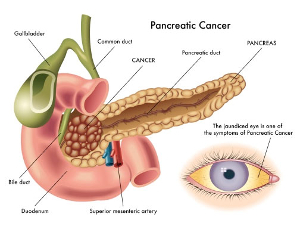
If your jaundice is not caused by an infection, you may have symptoms such as weight loss or itchy skin (pruritus). If the jaundice is due to pancreatic or biliary tract cancers (Refer: picture of anatomy of digestive system), the most common symptom you will experience is abdominal pain. Sometimes, you may have jaundice due to liver disease if you have:
- Chronic hepatitis
- Acute hepatitis B or C
- Polyarthralgias (inflammation of the joints)
What causes jaundice?
 Jaundice is a visible sign of an underlying disease process and not a single entity disease as many tend to assume.
Jaundice is a visible sign of an underlying disease process and not a single entity disease as many tend to assume.
It can be caused by infection with various types of viruses ( Hepatitis A, B, C, D & E) and bacteria or blood disorders or medical conditions that affect the normal metabolism of excretion of bilirubin. Some congenital enzyme deficiencies also can cause jaundice which rarely requires treatment. Excess copper and heavy metals and over usage of certain medicines including some herbal products may damage the liver to manifest as jaundice. Sometimes Jaundice may be the manifestation of an underlying cancer of biliary system or pancreas, an organ of digestive system that is situated close to the bile duct.
What is rat jaundice?
 The organism in the picture is called Leptospirosis bacterium. The infection that causes jaundice is spread by rats and hence some call it by this name. The severity of disease varies. Some times Leptospirosis can lead to kidney damage, meningitis (inflammation of the membrane around the brain and spinal cord), liver failure, respiratory distress, and even death.
The organism in the picture is called Leptospirosis bacterium. The infection that causes jaundice is spread by rats and hence some call it by this name. The severity of disease varies. Some times Leptospirosis can lead to kidney damage, meningitis (inflammation of the membrane around the brain and spinal cord), liver failure, respiratory distress, and even death.
What are the other causes of jaundice?
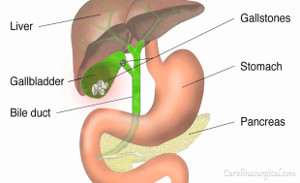
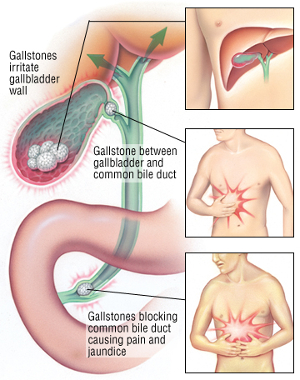 Stones in the biliary ducts can cause jaundice and severe pain. Stones obstruct the flow of bile resulting in jaundice, which is different from infective jaundice.
Stones in the biliary ducts can cause jaundice and severe pain. Stones obstruct the flow of bile resulting in jaundice, which is different from infective jaundice.
Cancer in bile duct or pancreas can also cause jaundice by obstruction to outflow of bile. To differentiate various causes of the obstructive jaundice higher end imaging by MRI study may be required.
Is Jaundice due to stones curable?
 Jaundice due to stones is curable. In the pre endoscopic days, say two to three decades ago, surgery was the only option. But now in majority of cases surgery may not be required and the stones from the bile ducts are extracted by endoscopic techniques – Endoscopic Retrograde Cholangio Pancreatography (ERCP)- to relieve the obstruction to outflow of bile. These techniques are technology oriented and require lot of expertise and training on the part of doctors.
Jaundice due to stones is curable. In the pre endoscopic days, say two to three decades ago, surgery was the only option. But now in majority of cases surgery may not be required and the stones from the bile ducts are extracted by endoscopic techniques – Endoscopic Retrograde Cholangio Pancreatography (ERCP)- to relieve the obstruction to outflow of bile. These techniques are technology oriented and require lot of expertise and training on the part of doctors.
What is Bilirubin?
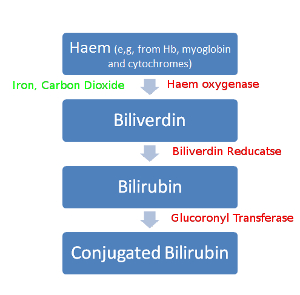 Bilirubin is derived from the haemoglobin, the pigment content of red blood cells released from the red blood cells (RBC) that under go daily breakdown and destruction as they grow older (normal life of RBCs is about 120 days). This pigment is metabolized and excreted by the liver. Any interference to the mechanisms of metabolism, excretion and obstruction to the out flow of the bile can cause Jaundice by depositing the excess bilirubin, in the body tissues to give yellow colour.
Bilirubin is derived from the haemoglobin, the pigment content of red blood cells released from the red blood cells (RBC) that under go daily breakdown and destruction as they grow older (normal life of RBCs is about 120 days). This pigment is metabolized and excreted by the liver. Any interference to the mechanisms of metabolism, excretion and obstruction to the out flow of the bile can cause Jaundice by depositing the excess bilirubin, in the body tissues to give yellow colour.
Can a new born baby have jaundice?
 Noticing of Jaundice in the new born is common. Babies have a high level of red blood cells in their blood, which are broken down and replaced frequently. The liver in newborn babies is also not fully developed, so it’s less effective at removing the bilirubin from the blood. This is called physiological jaundice, which means not a disease.
Noticing of Jaundice in the new born is common. Babies have a high level of red blood cells in their blood, which are broken down and replaced frequently. The liver in newborn babies is also not fully developed, so it’s less effective at removing the bilirubin from the blood. This is called physiological jaundice, which means not a disease.
By the time a baby is about two weeks old, the liver is more effective at processing bilirubin. So jaundice often corrects itself by this age without causing any harm.
Less commonly, jaundice can be due to birth disorders where the bile ducts are abnormally narrow (biliary atresia) or parents Rh blood group incompatibility. These can be addressed by specialists.
How is jaundice related to Blood disorders?
Jaundice can be caused by the excessive destruction of red blood cells from various blood disorders. This rapid increase in bilirubin levels in the bloodstream overwhelms the liver’s capability to properly metabolize the bilirubin, and consequently the levels of unconjugated bilirubin increase. Conditions which can lead to an increase destruction of red blood cells include Malaria, Sickle cell disease, Hereditary spherocytosis, Thalassemia, drugs, autoimmune disorders.
Can alcohol cause jaundice?
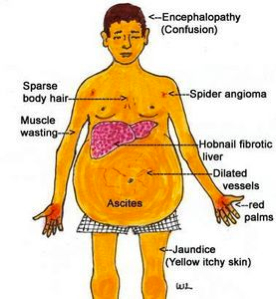 Alcoholic hepatitis is most likely to occur in some people who drink heavily over many years and this may lead to a condition called cirrhosis with impaired capacity of liver. People who continue to drink alcohol face a high risk of serious liver damage Characterised by excess fluid in the abdomen (ascites) causing a pot belly, wasting of muscles, swelling of legs and general decline in health, progressing to jaundice, kidney and liver failure and death.
Alcoholic hepatitis is most likely to occur in some people who drink heavily over many years and this may lead to a condition called cirrhosis with impaired capacity of liver. People who continue to drink alcohol face a high risk of serious liver damage Characterised by excess fluid in the abdomen (ascites) causing a pot belly, wasting of muscles, swelling of legs and general decline in health, progressing to jaundice, kidney and liver failure and death.
Which type of jaundice doesn’t need any treatment?
No treatment for jaundice? Sounds unbelievable?
Yes, there are some genetic liver disorders where bilirubin levels are elevated in the bloodstream. But this normally has no serious consequences, although mild jaundice may appear under conditions of exertion or stress. The cause of this hyperbilirubinemia is the reduced activity of the enzyme which helps in the processing of bilirubin by the liver.
Gilbert’s syndrome and Crigler-Najjar
syndrome are such genetic liver disorders which require only periodic monitoring. Once the diagnosis is established, no specific treatment is needed.
But my neighbour was told to undergo surgery for jaundice? Why?
When there is obstruction to the normal flow of bile from the liver into the intestine, jaundice arises due to increased levels of conjugated bilirubin in the bloodstream. This jaundice due to outflow obstruction is called surgical jaundice. The liver function may be normal in the early phase.
Physical disruption to outflow of bile may be caused by such conditions as gallstones, cancer (pancreatic cancer, gallbladder cancer and bile duct cancer), strictures of the bile ducts, cholangitis, pancreatitis, and parasites (for example, liver flukes), which cause jaundice. Here the treatment aims to remove the obstruction by either laparoscopic surgery or endoscopic management if feasible. If done successfully it provides relief. In inoperable conditions jaundice relief is provided by endoscopic techniques by introducing ‘stents’. This is purely a palliative measure
What if there is Jaundice?
Any adult who develops jaundice needs to undergo a comprehensive medical evaluation to identify the cause of jaundice. If the underlying liver disease is hepatitis often caused by infections, investigations aim to identifying the infecting agent for initiating suitable medical treatment.
But if the jaundice is caused by obstruction to the outflow of bile by either gallstones or a stricture or a cancer tumour sitting across the path of bile flow, suitable imaging studies are undertaken. And if the obstruction is found operable, surgical management is offered.
How can I prevent jaundice?
Since there are many causes of jaundice, it is hard to provide specific prevention measures. Some general tips include:
- Avoid hepatitis infection by hygiene and appropriate immunisation
- Avoid excess alcohol and stay within limits
- Maintain a healthy weight
- Manage your cholesterol
What is my diet in Jaundice?
If the jaundice is due to viral infection, fats and oils shall be avoided and foods rich in carbohydrates are advised. ( Refer to Diet Section)
Abdominal Pain
Just about everybody at one point or another will experience abdominal pain. Most of the causes are not serious and can be readily diagnosed and treated. However, pain can also be a sign of a serious illness. It’s important to be able to recognize symptoms that are severe and know when to call a doctor.
What Are the Most Common Causes of Abdominal Pain?
Whether it’s a mild stomach ache, sharp pain, or stomach cramps, abdominal pain can have numerous causes. Some of the more common causes include:
Indigestion, Gastroesophageal reflux disease (GERD), Constipation, Irritable bowel syndrome (IBS), Food allergies, Lactose intolerance, Appendicitis, Menstrual cramps, Peptic ulcer, Gallstones, Kidney stones, Crohn’s disease, tuberculosis of abdomen, Urinary tract infection, Pelvic inflammatory disease.
How Is the Cause of Abdominal Pain Determined?
There are many potential causes of abdominal pain. Your doctor will perform a thorough physical examination. Once clinical examination has been completed you undergo some tests to help find the cause of your pain. These may include stool or urine tests, blood tests, barium swallows or enemas, an endoscopy X-ray, ultrasound study(US), or CT scan.
How Is Abdominal Pain Treated?
Treating abdominal pain depends on its cause. Treatments can range from medications for inflammation, GERD or ulcers, to antibiotics for infections, to changes in personal behaviour for abdominal pain caused by certain foods or beverages. In some cases, such as appendicitis and a hernia, surgery may be necessary.
Swollen Legs and Ankles
There are many potential causes of foot, leg, and ankle swelling. They include certain lifestyle conditions or medications, such as:
- being overweight
- standing for prolonged periods of time
- being confined for long periods of time (especially during long car rides or flights)
- Drugs- hormones, blood pressure medications, nonsteroidal anti-inflammatory drugs (NSAIDs)
Natural changes during a woman’s menstrual cycle & pregnancy
Medical conditions that can cause swelling of legs
A blood clot of the leg, an infection in the leg area, venous insufficiency, pericarditis (a swelling of the membrane around the heart), organ failure -particularly the heart, liver, or kidney, injury, recent pelvic surgery,
lymphedema (a condition that causes blockages in the lymph system)
cirrhosis of liver.
What are the alarming ( Red Alert) symptoms?
Commonly encountered alarm symptoms related to digestive system are:
dysphagia (difficulty swallowing); odynophagia (painful swallowing); gastrointestinal bleeding or anemia; weight loss; and chest pain.
Dysphagia in combination with GERD usually signifies a peptic stricture or achalasia cardia but can also be present in esophageal malignancies.
If you have any of these symptoms, you shall visit your doctor for appropriate management.
These are the most common digestive diseases
- Gastroesophageal Reflux Disease (GERD)
- Achalasia (Difficulty in swallowing)
- Peptic ulcer disease
- Hepatitis – Acute and chronic
- Alcoholic liver Disease
- Gallstone Disease
- Pancreatitis –Acute and Chronic
- Irritable Bowel syndrome (IBS)
- Inflammatory Bowel Disease -Crohn’s disease & Ulcerative colitis
- Diarrhoea- Acute & Chronic
- Appendicitis
- Cancer
Chest Pain or Heart burn: Gastroesophageal Reflux Disease (GERD)
When stomach acid backs up into the oesophagus — a condition called acid reflux — you may feel a burning pain in the middle of your chest. It often occurs after meals or at night.
While it’s common for people to experience acid reflux and heartburn once in a while, having symptoms that affect your daily life or occur at least twice in a week could be an indication of GERD, a chronic digestive disease that affects 20 percent of population.
When should you consult a doctor?
If you experience persistent heartburn, bad breath, tooth erosion, nausea, pain in your chest or upper part of your abdomen, or have trouble swallowing or breathing, see your doctor.
What will the doctor do?
Apart from routine blood tests, an ultrasound study and endoscopy may be ordered to examine the interiors of your food pipe and stomach.
How can I avoid these symptoms?
Most people find relief by avoiding the foods and beverages that trigger their symptoms or by taking antacids or other medications that reduce stomach acid production and inflammation of the oesophagus. However, some cases of GERD may require treatment, such as weeks long medication or even surgery if the symptoms are unrelenting.
Achalasia
What is achalasia?
Achalasia is a rare disorder of the oesophagus. It is characterized by enlargement of the oesophagus, impaired ability to push food down toward the stomach (peristalsis), and failure of the muscle at the lower part of the esophagus, the lower esophageal sphincter (LES), to relax. It is the contraction and relaxation of the sphincter that moves food through the tube.
What is the treatment for Achalasia?
Treatment options and recommendations are as follows:
- Initial therapy choice should be based on patient age, sex, preference, and local institutional expertise
- Pharmacologic therapy consisting of of nitrates and calcium channel blockers are most commonly used for patients
- Graded pneumatic dilation (PD) is considered in some cases
- Surgical myotomy by Per Oesophageal Endoscopic Myotomy ( POEM) is the latest procedure where the offending constriction is divided by endoscopy. Earlier the same was accomplished laparoscopically.
- Botulinum toxin therapy is recommended for patients not suited to PD or surgery.
Peptic Ulcer Disease
What Are Peptic Ulcers?
Peptic ulcers are sores that develop in the lining of the stomach, lower esophagus, or small intestine (the duodenum), usually as a result of inflammation caused by the bacteria H. pylori, as well as from erosion from stomach acids. Peptic ulcers are a fairly common health problem.
Ulcer in the stomach and duodenum (first portion of small intestine) can cause pain in the abdomen and symptoms of indigestion.
What are the causes of peptic ulcers?
Smoking, drinking too much alcohol, frequent use of aspirin, ibuprofen, and other anti-inflammatory drugs, radiation therapy, Helicobacter pylori (H. pylori), a bacteria that can cause a stomach infection and inflammation, stomach cancer.
What are the symptoms of peptic ulcers?
The most common symptom of a peptic ulcer is burning abdominal pain that extends from the navel to the chest, which can range from mild to severe. In some cases, the pain may wake you up at night.
Other common signs of a peptic ulcer include changes in appetite, nausea, bloody or dark stools (melena), unexplained weight loss, indigestion, vomiting, chest pain.
What are the tests done for Peptic Ulcers?
Endoscopy establishes diagnosis. Upper GI Endoscopy (OGD)
In this procedure, your doctor inserts an endoscope down your throat and into your stomach and small intestine the area for ulcers. This instrument also allows your doctor to examine the interiors and remove tissue samples for examination.
How to Treat a Peptic Ulcer?
Treatment will depend on the underlying cause of your ulcer. If tests show that you have an H. pylori infection, your doctor will prescribe a combination of medication, which you will have to take for up to two weeks. The medications include antibiotics to help kill infections, and proton pump inhibitors (PPIs) to help reduce stomach acid.
You may experience minor side effects like diarrhea or upset stomach from antibiotic regimens.
What are the complications of peptic ulcers?
Untreated ulcers can become worse over time and lead to a host of serious health complications which may require hospitalization and even emergency proceudres or surgery. The complications are perforation, a hole develops in the lining of the stomach or duodenum, Internal bleeding, a potential life threatening condition if not treated adequately. Outlet obstruction due to Scar tissue makes it difficult for food to pass through your digestive tract. Signs of scar tissue include vomiting and weight loss. Seek urgent medical attention if you experience the following symptoms:
- Sudden, sharp abdominal pain
- Fainting, excessive sweating, or confusion, as these may be signs of shock
- Blood in vomit or stool
- Abdomen that’s hard to the touch
Hepatitis
What Is Hepatitis?
Hepatitis refers to an inflammatory condition of the liver. It’s commonly caused by a viral infection, but there are other possible causes of hepatitis. These include autoimmune hepatitis and hepatitis that occurs as a secondary result of alcohol, drugs, toxins, and medications. Autoimmune hepatitis is a disease that occurs when your body produces antibodies against your own liver tissue due to mistaken identification.
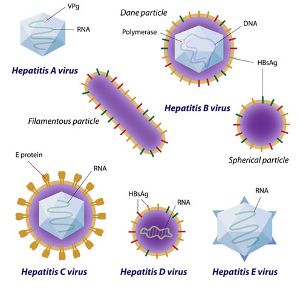
Viral Hepatitis is most common inflammation of the liver, caused by a viral infection. There are five main hepatitis viruses, referred to as types A, B, C, D and E.
These five types are of greatest concern because of the burden of illness and death they cause and the potential for outbreaks and epidemic spread.
Note : On Acute viral hepatitis & jaundice see the section with same name under Digestive Symptoms.
Acute Alcoholic Liver Disease
What is alcoholic liver disease (ALD)?
ALD is the development of liver damage as a result of heavy alcohol drinking. This damage may result in three patterns: fatty liver (an abnormal accumulation of fat in the liver), alcoholic hepatitis and cirrhosis (progressive destruction and regeneration of liver cells with fibrotic connective tissue).
What causes ALD?
Heavy consumption of alcohol (20-40 grams per day) is the major cause of ALD
What are the symptoms of ALD?
Some patients with ALD may be asymptomatic while others may present with a wide range of symptoms such as nausea, retching, diarrhea, anorexia, abdominal pain, liver enlargement. Others may seek medical attention because of the effects of alcoholism that may include inappropriate social behaviors, accidents, depression, tremors.
What is “fatty liver”?
Fatty liver is an abnormal accumulation of fat (small or large droplets) in the cytoplasm of liver cells and may often be accompanied by fibrosis. Conditions other than heavy alcohol consumption may also cause fatty liver.
Fatty liver is present in approximately 90 to 100 percent of heavy drinkers
What is alcoholic hepatitis and how is it diagnosed?
Alcoholic hepatitis is an inflammation of the liver characterized by necrosis and fibrotic scarring. The definitive diagnosis of alcoholic hepatitis is made by liver biopsy. Other considerations in diagnosis include a history of chronic or current heavy alcohol consumption, an enlarged liver and blood enzyme analysis. Patients with alcoholic hepatitis may present with anorexia, nausea, jaundice and weight loss.
What is alcoholic cirrhosis?
Alcoholic cirrhosis is a liver disease, characterized by widespread destruction and regeneration of liver tissue with marked increase in fibrotic connective tissue. The regenerated liver tissue forms nodules and permanently alters the structure of the liver. The scarring and increased connective tissue results in impairment of liver function. Continued necrosis (death) and fibrosis result in a progressive deterioration and ultimately end-stage liver disease.
Which tests and procedures are done to diagnose ALD?
Blood tests are useful in the determination of ALD. Blood tests can establish alcohol as the cause of the disease Serum electrolytes, mean corpuscular volume (MCV) and serum uric acid levels are also indicative of ALD in combination with results from other tests. Prothrombin time (ability of the blood to clot) may be indicative of mild hepatic disease, but may be present in hepatic failure.
Abdominal ultrasound and CT scanning may also be performed. Abdominal ultrasound is useful in the assessment of fatty content of the liver. CT scanning detects cirrhosis, portal hypertension and tumors.
What is a liver biopsy and will such a procedure require hospitalization?
A liver biopsy is usually performed in a hospital or a GI clinic. After a sedative and local anesthetic is administered, a needle is inserted through the skin and into the body of the liver. Small pieces of liver tissue are extracted for microscopic examination.
How is ALD treated?
The most important aspect of treatment in ALD is the immediate and total abstinence from alcohol. It is also critical that the patient’s nutritional intake is adjusted to maintain a high-calorie, high-protein diet.
Hospitalization may be necessary for those patients who have extrahepatic complications. Drugs may be used to treat the symptoms of withdrawal. Proteins and vitamin dietary supplements are prescribed. Vitamin B and K are administered. Potassium, magnesium and zinc are administered to those patients with decompensated liver disease. Orthotopic liver transplantation improves survival rates in decompensated liver cirrhosis.
What are the complications of ALD?
Complications of ALD are usually caused by the systemic complications of hepatic injury.
portal hypertension- an obstruction of the normal blood flow through the liver and reduction in functional hepatocyte mass. Due to poor synthetic ability of liver to produce albumin (a protein responsible for maintaining serum osmotic pressure) the resultant hypoalbuminemia may cause the formation of ascites, the accumulation of serous fluid in the abdomen. These conditions may occur in those with alcoholic hepatitis or alcoholic cirrhosis and in other non-alcohol related liver diseases.
Varices-Blood flow through alternative pathways result in the development of varices and hypersplenism. Spontaneous bacterial peritonitis may occur in the acutely ill cirrhotic patient
Reduction in functional liver mass causes hepatic encephalopathy ,mental dysfunction caused by an accumulation of nitrogenous wastes in the blood and brain, coagulopathy (dysfunctional clotting mechanism)
How are the complications of ALD treated?
The treatment for ascites is salt restriction and careful diuresis (fluid removal through the use of drugs that cause the patient to excrete large volumes of urine). Paracentesis (aspiration of fluid from the abdominal cavity) is reserved for symptomatic patients with tense ascites (respiratory distress, abdominal pain and early satiety).
How are varices treated?
Therapy for variceal bleeding includes prompt fluid replacement and medication to lower portal pressure. Endoscopic therapy may be employed to stop bleeding. Oesophageal varices are usually managed by endoscopic variceal banding and/or sclerotherapy.
How is hepatic encephalopathy managed?
Hepatic encephalopathy is treated by correcting the precipitating event and by the administration of drugs that promotes the elimination of ammonia and an antibiotic may also be administered. It works by killing the intestinal bacteria that degrade proteins to ammonia and amines which are toxic for brain. Coagulopathy is treated by administration of vitamin K, fresh frozen plasma and if required blood. Liver transplantation may ultimately be the only way to correct this problem.
Hypoalbuminemia can be treated with IV albumin replacement. Although this is a short-term, expensive treatment, it can help mobilize ascites and increase serum albumin.
What lifestyle changes one need to make?
The most important lifestyle change is total abstinence from alcohol. Hepatic improvement may occur if alcohol consumption is reduced when accompanied by nutritional supplementation.
How to Prevent Hepatitis?
Hygiene
Practicing good hygiene is one key way to avoid contracting hepatitis. If you’re traveling you should avoid:
- Drinking public tap water
- Ice
- Seafood
- Raw fruit and Vegetables
Hepatitis contracted through contaminated blood can be prevented by:
- Not sharing drug needles
- Not sharing razors
- Not using someone else’s toothbrush
- Not touching spilled blood
- Vaccination
Hepatitis B Prophylaxis
Primary Vaccination:
Viruses that primarily attack the liver are called hepatitis viruses. There are several types of hepatitis viruses including types A, B, C, D, E, and possibly G. Types A, B, and C are the most common. Viral hepatitis types B and C can cause chronic hepatitis (long standing disease).
Hepatitis A is a liver infection caused by the Hepatitis A virus (HAV). Hepatitis A is highly contagious. It is usually transmitted by the fecal-oral route, either through person-to-person contact or consumption of contaminated food or water. Hepatitis A is a self-limited disease that does not result in chronic infection. The best way to prevent Hepatitis A is by getting vaccinated.
Hepatitis B is a serious disease caused by a virus that attacks the liver. The virus, which is called hepatitis B virus (HBV), can cause lifelong infection, cirrhosis (scarring) of the liver, liver cancer, liver failure, and death. It is a major global health problem. Hepatitis B vaccine is available for all age groups to prevent HBV infection.
The vaccine is made using recombinant DNA technology and contains only a portion of the outer protein coat of the virus, called the hepatitis B surface antigen. The vaccine is a very safe and effective immunization against a Hepatitis B viral infection.
Experts are currently developing vaccines against hepatitis C, D, and E.
The Vaccination Schedule
Hepatitis B Vaccine
| Age Group | Dose | Volume | Doses | Schedule |
|---|---|---|---|---|
| 0-19 years | 5mcg | 0.5ml | 3 doses | 0, 1 and 6 months |
| ≥ 20 years | 10mcg | 1.0 ml | 3 doses | 0, 1 and 6 months |
| Pre & Post Dialysis Patients | 40mcg | 1.0 ml | 3 doses | 0, 1 and 6 months |
Hepatitis A Vaccine
| Age | Dose | Volume | Doses | Schedule |
|---|---|---|---|---|
| 1-18 years | 720 ELISA UNITS | 0.5ml | 2 doses | 0,6-12 MONTHS |
| ≥ 19 years | 1440 ELISA UNITS | 1.0 ml | 2 doses | 0,6-12 MONTHS |
Gallstone Disease
Other name : biliary calculi
Gallstones are rounded faceted solid deposits in the gallbladder or bile ducts. These range from a few millimetres to centimetres in diameter. The most commonly found gallstones are comprised of a mixture of cholesterol and calcium salts. Some are pure cholesterol, but many are mixed. A small number are called “pigment” stones and contain bilirubin salts. Gallstones may be associated with chronic infection in the gallbladder (Cholecystitis).
What are the symptoms of gallstones?
Gallstones may or may not produce symptoms. But they cause pain when they are stuck in the neck of gallbladder or passed through the bile ducts or when there is infection. Some attribute chronic dyspeptic symptoms to presence of gallstones.
How is the diagnosis of gallstones made?
A plain abdominal x-ray may show calcified gallstones in 20% of patients. But ultrasound is the method of choice to diagnose gallstones, but Magnetic Resonance Cholangiography or CT may also be ordered.
Is there medical treatment?
The main stay of treatment is surgery- either laparoscopic or open depending on the condition of the patient and the GB. Asymptomatic stones less than 5 mm may be treated with ursodeoxycholoic acid tablets may be tried for the dissolution of small to medium sized radiolucent, cholesterol-rich gall-stones in patients with a functioning gall bladder. But the duration of treatment may be 6 months and the side effects of medication make it unpredictable.
Acute cholecystitis
What is cholecystitis?
Acute cholecystitis is swelling and inflammation of the gallbladder. It is a potentially serious condition that needs to be treated in a hospital.
What are the symptoms?
Typically, the pain starts in the upper right side of your abdomen (tummy) that spreads towards your right shoulder. Breathing deeply can make the pain worse.
You may have additional symptoms such as fever, nausea and vomiting, loss of appetite and jaundice.
What causes acute cholecystitis?
Acute cholecystitis can be grouped into calculous cholecystitis and acalculous cholecystitis.
Calculous cholecystitis
Calculous cholecystitis is the most common. It develops when the cystic duct that drains the gallbladder (GB), gets blocked by a gallstone or biliary sludge. The blockage in the cystic duct results in inflammation and infection by bacteria.
Acalculous cholecystitis
There is no stone to obstruct the cystic duct in acalculous cholecystitis. It is less common but usually more serious type of acute cholecystitis. It usually develops as a complication of a serious illness, sepsis or injury that damages the gallbladder.
How is Cholecystitis diagnosed?
On clinical examination, when a hand is pressed just below your rib cage you will experience sudden pain as your gallbladder reaches your doctor’s hand on deep breathing.This is further corraborated with tests which may include:
Blood tests, an ultrasound scan of your abdomen to check for gallstones. Imaging such as an X-ray, a CT or an MRI scan -Magnetic Resonance Cholangio Pancreatography (MRCP)– may also be carried out..
What is the treatment of Cholecystitis?
The treatment of Cholecystitis is surgical removal of the gallbladder, known as cholecystectomy.
Why not remove the stones alone rather than the entire GB?
If stones alone are removed, they will form again because the gallbladder is diseased and there is a tendency to form stones and recurrence of problem.
Doesn’t removal of GB affect my digestion and health?
No harm is done by removing a diseased GB. After a successful surgery, loss of GB will not pose any health related problems. Cholecystectomy for stone disease is the standard scientific treatment world over and a time tested procedure over more than a century.
In analogy, it’s like dismantling a rusted and leaky overhead water tank. Not to worry as long as the plumbing to supply the water is intact.
How is cholecystectomy done? Is it painful?
Cholecystectomy is carried out under general anaesthesia, using either a ‘Laparoscopic’ or ‘open’ technique. Laparoscopic cholecystectomy is the gold standard now.
Both techniques are usually carried out under general anaesthesia, so the person undergoing the operation is asleep during surgery and will feel no pain. Post operatively any minimal pain responds to medication.
What is laparoscopic surgery?
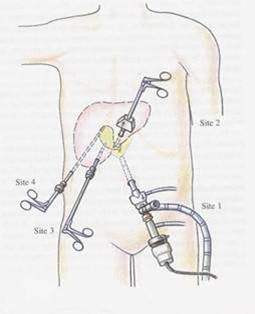 During laparoscopic cholecystectomy, the surgeon makes four small incisions in your abdomen. A tube with a tiny video camera is inserted into your abdomen through one of the incisions. Your surgeon watches a video monitor in the operating room as special surgical instruments are inserted through the other incisions in your abdomen and your gallbladder is removed.
During laparoscopic cholecystectomy, the surgeon makes four small incisions in your abdomen. A tube with a tiny video camera is inserted into your abdomen through one of the incisions. Your surgeon watches a video monitor in the operating room as special surgical instruments are inserted through the other incisions in your abdomen and your gallbladder is removed.
How does Laparoscopic surgery differs from open surgery?
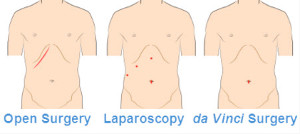 In the laparoscopic surgery 4 small cuts ( about 5-10mm) are made in your abdomen, through which special surgical instruments are inserted to access the GB. Scars will not be obviously visible and recovery is fast.
In the laparoscopic surgery 4 small cuts ( about 5-10mm) are made in your abdomen, through which special surgical instruments are inserted to access the GB. Scars will not be obviously visible and recovery is fast.
In ‘Open’ surgery practiced earlier times, a single larger cut is made in the abdomen to access the GB . The hospital stay and recovery are much longer. This method is preferred in delayed cases when the GB has burst or laparoscopic access is difficult.
How long does it take to recover from laparoscopic surgery?
Recovery is fast in the case of timely surgery. In uncomplicated cases feeds are started the next day or two following surgery. You are ready to go home by 2nd or 3rd post operative day. Associated medical diseases like diabetes or heart disease etc. may at times delay discharge to home.
After how long can I do strenuous work following cholecystectomy?
Normal office work or domestic chores can be resumed in a couple of weeks. Strenuous work may be avoided for 3-4 weeks.
How can I prevent acute cholecystitis?
It’s not always possible to prevent acute cholecystitis, but you can reduce your risk of developing the condition by cutting your risk of gallstones. Adopting a healthy, balanced diet and reducing the number of high-cholesterol foods you eat, as cholesterol is thought to contribute to the formation of gallstones, is the main step.
What if I have gallstones in my bile duct also?
The gallstones in the bile duct need to be removed first by ERCP followed by cholecystectomy. These are two separate procedures done with an interval of a day or two or more depending on the disease condition.
How long do I have to stay in the hospital?
People are often able to walk and feed the next day as their surgery, a two or three-night stay in the hospital is needed. In general, you can expect to go home once you’re able to eat and drink without pain and are able to walk unaided. It takes about a week to fully recover.
Will I have any side effects after removal of gallbladder (GB)?
Normally, the gallbladder collects and concentrates bile, releasing it when you eat to aid the digestion of fat. When the gallbladder is removed, bile flow remains unaffected.
How soon after surgery can the patient shower or bathe?
The patient may shower/bathe 3 days after surgery, providing he/she carefully protects the wounds after every quick shower/bath. No medication or ointments need to be applied. A touch of after shave lotion may not do harm.
How soon after surgery can the patient resume exercise or play sport?
Under normal circumstances the patient should be able to resume exercise and play sport within a month after surgery, provided he/she avoids strenuous physical activity.
Is there a gallbladder removal diet I should follow?
There isn’t a specific gallbladder removal diet that you should follow, but there are a few things you might consider.The amount of fat you eat at one time also plays a role. Avoid high-fat foods, larger amounts of fat can remain undigested and cause gas, bloating and diarrhoea. Increase the fibre in your diet. This can help normalize bowel movements. Eat smaller, more-frequent meals
Finally, how safe Is laparoscopic cholecystectomy?
Laparoscopic cholecystectomy is currently considered the “gold standard” for the surgical treatment of gallstone disease by all international societies for surgery.
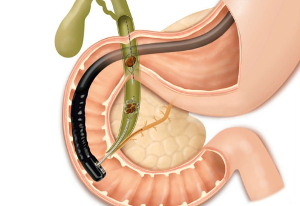
How are stones in the bile duct treated?
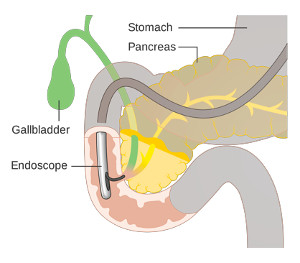 Gallstones in the bile duct are extracted by endoscopic Retrograde Cholangiopancreatography (ERCP) and endoscopic sphincterotomy. During this procedure, a balloon- or basket-type device is inserted into the bile duct under special X-Ray ( fluoroscopy) guidance and the stones are extracted.
Gallstones in the bile duct are extracted by endoscopic Retrograde Cholangiopancreatography (ERCP) and endoscopic sphincterotomy. During this procedure, a balloon- or basket-type device is inserted into the bile duct under special X-Ray ( fluoroscopy) guidance and the stones are extracted.
A cholecystectomy may be indicated at the same time or a later date.
What is biliary stenting?
If stones cannot be removed completely by ERCP or you have a history of some gallstones causing problems but do not wish to have your gallbladder removed, your doctor may place biliary stents (tiny tubes to open the passage). These will provide adequate drainage and help prevent spilling of stones into the bile duct ( Choledocholithiasis). The stents can also prevent cholangitis biliary sepsis (inflammation) and infection.
What if stones in the bile duct (CBD) is suspected?
If Stones in the CBD are are suspected, any or some of the following investigations may establish the diagnosis.
Ultrasound Study(US), Abdominal CT scan, Endoscopic ultrasound (EUS): an ultrasound probe is inserted on a flexible endoscopic tube and inserted through the mouth to examine the digestive tract Endoscopic retrograde cholangiography (ERCP), Magnetic resonance cholangiopancreatography (MRCP) Percutaneous Transhepatic Cholangiogram (PTCA).
What are the complications of untreated CBD stones?
Recurrent pain abdomen, fever, ever deepening jaundice and its effects such as severe itching. The Cholangitis- infection of bile ducts may lead to severe sepsis to end up in shock.
Pancreatitis
Acute Pancreatitis
What is acute pancreatitis?
Acute pancreatitis is an inflamtion of the pancreas, caused by the pancreas juices being caught in the pancreas, and self-digesting itself ( auto digestion). It occurs suddenly and may be mild, moderate or severe, depending on the amount of damage and organ dysfunction caused by the episode.
What causes acute pancreatitis?
Biliary stones alcohol intake are leading causes of acute pancreatitis. Several drugs like immunosuppressants may also cause pancreatitis. Pancreas divisum, a congenital defect of the pancreatic ducts, microscopic stones, metabolic imbalances (hyperlipidemia and hypercalcemia), sphincter of Oddi dysfunction, scorpion sting and trauma may also cause acute pancreatitis.Some viruses like hepatitis A, B, cytomegalovirus and mumps may also cause pancreatitis.
What are the symptoms of acute pancreatitis?
Abdominal pain, nausea and vomiting are the most frequent symptoms of acute pancreatitis. Fever, jaundice, hypotension and increased rate of heart beat tachycardia are not uncommon.
Can acute pancreatitis become chronic pancreatitis?
Yes. Chronic pancreatitis results when inflammation in the pancreas has caused damage and resulted in fibrosis, calcifications and ductal inflammation. It is also possible for patients with chronic pancreatitis to have episodes of acute pancreatitis.
How is acute pancreatitis diagnosed?
Elevated serum amylase and lipase (pancreatic enzymes) in the background of sudden onset of abdominal pain clinches diagnosis of acute pancreatitis.
Additional diagnostic tests like abdominal and chest X-rays, computed tomography (CT) scans, ultrasound studies, and endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS) are useful in detecting stones, strictures in the ducts, tumors, abscesses, pseudocysts or necrosis (death of tissue).
Can I prevent acute pancreatitis?
Avoiding known causes of pancreatitis like alcohol consumption may help prevent the onset of the disease.
What is the treatment of acute pancreatitis?
The treatment of acute pancreatitis depends on its severity.
If the disease is considered mild, the patient is usually fed intravenously and treated supportively with pain control medication, intravenous fluids and a nasogastric tube to relieve vomiting.
In case of severe pancreatitis the patient may be admitted to an intensive care unit. Antibiotics may be used to prevent sepsis. Therapeutic endoscopic retrograde cholangiopancreatography (ERCP) may be performed in the early stages of acute pancreatitis to remove gallstones and may require sphincterotomy.
Surgical debridement and drainage may be necessary if infected pancreatic necrosis (cell death) arises.
What are the possible complications from acute pancreatitis?
Complications include hypotension (drop in blood pressure), pulmonary edema and adult respiratory distress syndrome. Localized complications include fluid collections, pancreatic pseudocysts, pancreatic necrosis and infectious pancreatic necrosis.
Is there a hereditary link with acute pancreatitis?
No. There may, however, be genetic influence in chronic pancreatitis.
Chronic Pancreatitis
What is the difference between acute pancreatitis and chronic pancreatitis?
Acute pancreatitis is an isolated episode of abdominal pain accompanied by elevations in blood enzyme levels. Acute pancreatitis may lead to chronic pancreatitis. Chronic pancreatitis is a painful disease of the pancreas in which inflammation has resolved, but with resultant damage to the gland characterized by fibrosis, calcification and ductal inflammation. It is possible for patients with chronic pancreatitis to have episodes of acute pancreatitis.
What causes chronic pancreatitis?
The most common cause of chronic pancreatitis in Western societies is alcohol. Alcohol consumption has been implicated in approximately 70 percent of cases as a major cause of this disease. Other causes include gallbladder disease, hyperparathyroidism (increased secretion from the parathyroid glands) and trauma to the pancreas.
What are the symptoms of chronic pancreatitis?
Symptoms of chronic pancreatitis range widely from a sudden acute abdominal catastrophe to mild unremitting abdominal pain or episodes of deep epigastric pain, vomiting, constant dull, weight loss, steatorrhea and glucose intolerance. The pain of chronic pancreatitis often radiates to the back.
Diarrhea due to fat malabsorption may result in bulky, foul-smelling stools that may appear oily and float in the toilet basin (steatorrhea).
How is chronic pancreatitis diagnosed?
Chronic pancreatitis is best diagnosed clinical examination and history, serum enzymes, exocrine function and imaging studies (X-rays).
Are there any particular complications that result from chronic pancreatitis?
Yes. Nutrient malabsorption, diabetes mellitus and splenic vein thrombosis are common complications of chronic pancreatitis.
How is chronic pancreatitis treated?
Treatment for chronic pancreatitis includes medical, endoscopic and surgical therapy.Pancreatic enzyme replacement is therapy that replaces enzymes, the production of which is reduced because of the disease process of pancreatitis. These enzymes are critical to manage malabsorption. They are useful in significantly improving steatorrhea (passage of fat through the stool).
A stent, or endoprosthesis, is a hollow synthetic tube that may be inserted in a pancreatic or biliary duct or sphincter to facilitate flow of pancreatic juice or bile.
Endoscopic sphincterotomy may be done to treat disorders of the muscle or to facilitate endoscopic therapy in the biliary and pancreatic ducts.
Surgery for chronic pancreatitis is indicated when more conservative approaches, such as medical and endoscopic, fail to give relief from symptoms.
Can patients expect long-term relief of pain after surgery?
Surgical intervention provides long-term relief of pain in 70 percent of patients. When patients have exhausted other avenues of treatment for pain relief, surgery should be considered.
If I have chronic pancreatitis and am being treated, can I expect a full recovery from this disease?
The changes of chronic pancreatitis are not reversible. However, it is possible to have control of pain and steatorrhoea with medical, endoscopic or surgical treatment.
What is Irritable Bowel Syndrome (IBS)?
Irritable bowel syndrome (IBS) is a gastrointestinal disorder characterized by the presence of a cluster of symptoms in adults or children that include cramping, abdominal pain, increased gas, altered bowel habits, food intolerance, and bloating.
IBS is a “functional” disorder that refers to the changes in the functioning of the digestive system. This may cause a collection of symptoms referred to as IBS, meaning that it is a problem with the movement (motility) rather than any physical damage to the tissues of the digestive system.
What are the symptoms of IBS?
If you have stomach pain or discomfort at least three times a month for several months? It could be irritable bowel syndrome (IBS), another common digestive condition.
Ten to 15 percent of the population suffers from irritable bowel syndrome, according to the International Foundation for Functional Gastrointestinal Disorders. Signs of IBS can vary widely: You can be constipated or have diarrhoea, or have hard, dry stools on one day and loose watery stools on another. Bloating is also a symptom of IBS.
What causes IBS?
It isn’t known, but treatment of symptoms centres largely on diet.
How is IBS diagnosed?
IBS is diagnosed by a process of exclusion and never a clinical diagnosis. It means that if you have such symptoms as described above, you will be ordered investigations that include common laboratory blood and stool tests, imaging studies like ultrasound or CAT scan, Colonoscopy and biopsy etc. Sometimes more elaborate testing may be required if any of these tests are either inconclusive or leave a doubt on the possible cause. If none of these tests come positive for any specific organic cause or disease, your condition is likely to be called IBS, a functional disorder.
What do
How is IBS managed?
By avoiding common trigger foods (dairy products, alcohol, caffeine, artificial sweeteners and beans, cabbage, and other foods that produce gas), or following a low-fat diet that’s also high in fibre.
What is the role of probiotics?
Friendly bacteria, such as the probiotics found in curds, may also help you feel better. Stress can trigger IBS symptoms, so some people find cognitive-behavioural therapy or low-dose antidepressants to be useful treatments.
Inflammatory bowel disease (IBD)
Ulcerative Colitis
Ulcerative colitis is an inflammatory bowel disease(IBD).
What are the symptoms of IBD?
Rectal pain or bleeding or both, Loss of appetite, Weight loss, Urgency to defecate
Inability to defecate in spite of urgency, Severe tiredness, Fever.
Consult a doctor if you have some combination of the following symptoms:
- Persistent change in bowel habits (e.g., diarrhoea for several weeks)
- Frequent stools
- Abdominal pain
- Blood or mucus in the stool
- Diarrhoea that awakens you from sleep
- Unexplained fever lasting more than a day or two
Ulcerative colitis symptoms tend to come and go, with periods of remission between. A remission can last for months or years.
What is the cause of IBD?
If your immune system mistakes food or other materials for invaders, sores or ulcers develop in the colon’s lining. If you experience frequent and urgent bowel movements, pain with diarrhoea, blood in your stool, or abdominal cramps, visit your doctor.
How is it diagnosed?
Tests that may be used to help diagnose ulcerative colitis and rule out other conditions include:
- Blood tests to check for anemia and infection
- Stool analysis to evaluate for other illnesses that are similar to ulcerative colitis, such as infection with bacteria, parasites, and certain toxins
- Flexible sigmoidoscopy to view just the lower portion of the colon
- Colonoscopy, an endoscopic examination to view the inside of the entire colon and obtain tissue samples for study
- X-ray to look for serious complications
- Barium enema, in which the colon is filled with liquid barium before x-rays are taken ( rarely done these days)
- CT scan of the abdomen or pelvis to see how much of the colon is inflamed and whether serious complications have developed
Colonoscopy identifies the characteristic pattern of ulceration and mucosal changes in the colon. Biopsy establishes the diagnosis.
How is IBD treated?
IBD treatment consists of medication which can suppress the inflammation, and eliminating foods that cause discomfort. In severe cases, treatment for ulcerative colitis may involve surgery to remove the colon.
Crohn’s Disease
What is Crohn’s disease?
Crohn’s disease is part of a group of digestive conditions called inflammatory bowel disease (IBD). Crohn’s most commonly affects the end of the small intestine called the ileum, but it can affect any part of the digestive tract.
What causes this disease?
This chronic condition is an autoimmune disease, meaning that your immune system mistakenly attacks cells in your own body that it thinks are foreign invaders rather than own tissues. It is like the security you have appointed to protect you act against you !!
What are the symptoms of Crohn’s disease?
The most common Crohn’s symptoms are abdominal pain, diarrhoea, rectal bleeding, weight loss, and fever. Sometimes it may be confused with tuberculosis.
How is it diagnosed?
CT scan and enteroscopy and biopsy are the important tests to arrive at a diagnosis (Refer above).
Detailed history coupled with imaging studies identify the characteristic pattern of the disease to suspect the presence of disease. Endoscopic biopsy establishes the diagnosis.
Treatment depends on the symptoms and can include topical pain relievers, immunosuppressants, and very rarely surgery.
Appendicitis
What is appendicitis?
Appendicitis is a painful swelling of the appendix, the worm like appendage of large intestine, due to infection and inflammation.
What are the symptoms?
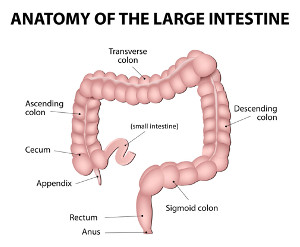 Typically pain starts in the middle of abdomen (tummy) that may come and go. It progresses within hours and the pain shifts to the lower right-hand side, where the appendix usually lies, and becomes constant and severe. Appetite is lost and makes you feel sick.
Typically pain starts in the middle of abdomen (tummy) that may come and go. It progresses within hours and the pain shifts to the lower right-hand side, where the appendix usually lies, and becomes constant and severe. Appetite is lost and makes you feel sick.
Who is affected?
Appendicitis is most common in young people from 10 to 20 years old but no age is bar. It can develop at any age.It is one of the commonest surgical emergencies.
What causes appendicitis? How can I prevent it?
It’s not exactly clear as to how appendicitis is triggered. Since it is not fully understood, there’s no guaranteed way of preventing appendicitis.
What is the treatment for appendicitis?
The treatment of appendicitis is surgical removal of the appendix, known as an appendicectomy done as soon as diagnosis is made.
What is appendicectomy? Is it painful?
Appendectomies are carried out under general anaesthesia, using either a ‘Laparoscopic’ or ‘open’ technique.
You will not feel any pain at all. It’s like going into deep sleep and getting up to know your surgery is over!
Laparoscopic or open surgery, which is better?
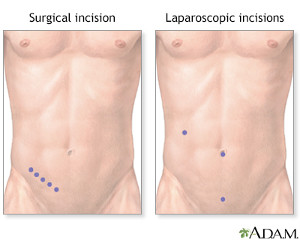 In the laparoscopic surgery 3 or 4 small cuts ( about 5mm) are made in your abdomen, through which special surgical instruments are inserted to access the appendix. Scars will not be obvious and recovery is relatively faster.
In the laparoscopic surgery 3 or 4 small cuts ( about 5mm) are made in your abdomen, through which special surgical instruments are inserted to access the appendix. Scars will not be obvious and recovery is relatively faster.
In ‘Open’ surgery, a single larger cut is made in the abdomen to access appendix . This is preferred when the appendix has burst or access is more difficult.
How long does it take to recover from surgery?
Recovery is fast in the case of timely surgery either by laparoscopic or open surgery. In uncomplicated cases feeds are started the next day or two following surgery.
After how long can I do strenuous work following appendicectomy?
Normal office work or domestic chores can be resumed in a couple of weeks. Strenuous work may be avoided for 3-4 weeks.
Isn’t removing the appendix harmful?
No one knows exactly why we have an appendix. Removing it is not harmful. And on the contrary, not removing an inflamed appendix can pose danger to life.
Piles, Fissure and Fistulectomy
What are haemorrhoids/piles?
In the inner lining of the anus there are three haemorrhoidal ‘cushions’ of tissue, which help to seal the anus and contribute to the control of the bowels
What are the symptoms of piles?
- Bright-red bleeding, Prolapse (haemorrhoid comes down when passing faeces), mucus discharge,
- Pain: Acute pain and the appearance of a lump protruding from the anus can be the result of thrombosis of the haemorrhoid, which is treated by surgery to relieve the discomfort.
What is Hemorrhoidectomy for Hemorrhoids
Haemorrhoidectomy is the surgery to remove haemorrhoids.
How painful is the surgery?
You will be given general anaesthesia or spinal anaesthesia so that you will not feel pain.
What happens to me after surgery?
The long-acting local anesthetic given right after the surgery gives relief of pain for 6 to 12 hours. You will stay overnight in the hospital after surgery, you will leave only after the anesthesia wears off and you have urinated. Inability to urinate sometimes occurs because of swelling (edema) in the tissues. Someone should drive you home.
What Care should I take after surgery
- Some bleeding is normal, especially with the first bowel movement after surgery.
- You can expect some pain after surgery. Please take prescription medicine for pain as prescribed.
What foods I can take?
For a few days after surgery, drink plenty liquids and eat a non spicy diet (plain rice and dhal, Idlis, Idiappams, bread and fruits like bananas ( if you are not a diabetic) papaya etc. You can return to regular foods in week time as you gradually increase the amount of fiber in your diet.
What about the wound care?
- Frequent soaks in warm water (sitz baths) help relieve pain and muscle spasms. You may apply numbing medicines Xylocaine ointment) before and after bowel movement to relieve pain.
- You take antibiotics as advised to prevent infection and reduce pain.
- You take stool softeners that contain fiber to help make your bowel movements smooth. Avoid straining.
When will I see my surgeon again?
Follow-up exams with the surgeon usually are done 4-5days after surgery to check for problems.
When can I expect total healing of wound and return to work?
Recovery takes about 2 to 3 weeks. Till that time, slight staining of under garments may happen. This should not cause any worry. Healing is always good after anal surgery. You can resume office work after 10 days. Strenuous and long hours of journey to be postponed for about 3 weeks.
Is Laser surgery better and less painful?
Lasers are often advertised as being a less painful, faster-healing method of removing haemorrhoids. But none of these claims have been proved. Lasers are more expensive than traditional techniques. The procedure takes longer, and it may cause deep tissue injury.
Fissure in Ano
What is Fissure in ano?
An anal fissure is a break or tear in the skin of the anal canal
What are the symptoms of piles?
May cause bright-red bleeding and acute pain during defaecation that may last for few hours.
What are the causes of anal fissure?
Constipation is the primary and sole cause of initiation of a fissure. Passage of hard stool, irregularity of diet, consumption of spicy and pungent food, faulty bowel habits, and lack of local hygiene can contribute for initiation of the pathology. In females, the ailment is usually triggered during pregnancy and following childbirth that may heal by itself or may progress to a chronic fissure.
What is the treatment of anal fissure?
Superficial fissures can be treated conservatively. The following are advised for simple fissures.
Warm water sitz baths soothes the pain and relaxes the spasm of the internal sphincter for some time
Stool softening is essential. Plenty of oral fluids also help in keeping the stools soft.
High-fiber-diet and bulk-forming agents such as Isaphgula; green leafy vegetables and fibrous fruits go a long way in increasing the bulk of stool. Application of local anesthetic cream or gel may help avoid the pain experienced in passage of stools.
Chronic fissure in ano : The above mentioned approaches do not prove effective in the chronic variety of fissures characterized by presence of an external skin tag. In such cases surgery is indicated. Partial division of internal sphincter fibers to relieve the sphincter spasm is presently considered the preferred surgical therapy
How painful is the surgery?
You will be given general anaesthesia or spinal anaesthesia so that you will not feel pain.
What happens to me after surgery?
The long-acting local anesthetic given right after the surgery gives relief of pain for 6 to 12 hours. You will to stay overnight in the hospital after surgery and may be a day more.
What Care should I take after surgery
Some spotting or bleeding is normal, especially with the first bowel movement after surgery.
If you experience pain after surgery, please take prescription medicine for pain as prescribed.
What about the wound care?
- Frequent sitz baths help relieve pain and muscle spasm. You may apply Xylocaine ointment before and after bowel movement to relieve pain.
- You take antibiotics as advised to prevent infection and reduce pain.
- You take stool softeners that contain fiber to help your bowel movements.
- Avoid straining.
What foods I can take?
For a few days after surgery, drink plenty liquids and eat a non-spicy diet (plain rice and dhal, Idlis, Idiappams, bread and fruits like bananas (if you are not a diabetic) papaya etc. You can return to regular foods in week time as you gradually increase the amount of fiber in your diet.
When will I see my surgeon again?
Follow-up exams with the surgeon usually are done 4-5days after surgery to check for problems.
When can I expect total healing of wound and return to work?
Healing is always good after anal surgery. You can resume office work after 7-10 days.
Fistula in ano
What is fistula in ano?
A fistula-in-ano is an abnormal communication between the anus and the perianal skin.
How does it occur?
Fistulas can occur spontaneously or secondary to a perianal abscess. In fact, following drainage of a perianal abscess, there is an approximate 50% chance of developing a chronic fistula. Fistulae may develop secondary to Crohn’s disease, anal fissures, carcinoma, radiation therapy, and tuberculosis infections.
How do I know I have fistula in ano?
Patients with Fistula-in-Ano present with chronic drainage of pus or stool from the skin opening beside the anal orifice. The discharge doesn’t heal on its own.
How is it diagnosed?
Physical exam remains the mainstay of diagnosis. Rectal examination is usually required. In some cases where there is a doubt about the extent or in case of multiple fistulous openings, an MRI fistulogram may be required to map the trajectory of the fistula for appropriate management.
What is the treatment for fistula in ano?
Excision of the fistula or the laying open technique -fistulotomy are useful in the management of majority of fistulae. The fistulectomy wound is not closed and allowed to heal by secondary intention.
How painful is the surgery?
You will be given general anaesthesia or spinal anaesthesia so that you will not feel pain.
What happens to me after surgery?
The long-acting local anesthetic given right after the surgery gives relief of pain for 6 to 12 hours. You will to stay overnight in the hospital after surgery and may be a day more.
What Care should I take after surgery
Some spotting or bleeding is normal, especially with the first bowel movement after surgery.
If you experience pain after surgery, please take prescription medicine for pain as prescribed.
What about the wound care?
- Frequent sitz baths help relieve pain and muscle spasm. You may apply Xylocaine ointment before and after bowel movement to relieve pain.
- You take antibiotics as advised to prevent infection and reduce pain.
- You take stool softeners that contain fiber to help your bowel movements.
- Avoid straining.
What foods I can take?
For a few days after surgery, drink plenty liquids and eat a non-spicy diet (plain rice and dhal, Idlis, Idiappams, bread and fruits like bananas (if you are not a diabetic) papaya etc. You can return to regular foods in week time as you gradually increase the amount of fiber in your diet.
When will I see my surgeon again?
Follow-up exams with the surgeon usually are done 4-5days after surgery to check for problems.
When can I expect total healing of wound and return to work?
Healing is always good after anal surgery. You can resume office work after 7-10 days. Complete healing may take 3-4 weeks.
Apart from clinical examination laboratory investigations of stool, blood tests, imaging studies consisting of chest x-ray, ultrasound study, CT scan and an MRI scan are required to assist in arriving at a diagnosis. Endoscopy affords direct examination of the internal architecture of hollow organs.
Oesophago GastroDuodenal Endoscopy (OGD)
What is OGD or Upper Gastrointestinal (UGI) Endoscopy?
Upper gastrointestinal endoscopy also called OGD, is a commonly performed procedure allowing direct visual examination of the inside of the upper gastrointestinal tract -oesophagus, stomach and duodenum using a flexible endoscope. The endoscope transmits the images electronically and viewed on a monitor.
What is the purpose of Gastroscopy?
Gastroscopy has many purposes. It allows an examination of the upper gastrointestinal tract for investigating and accurately identifying the abnormalities like gastritis, peptic ulcers polyps and cancer, which may be captured on a photograph. This procedure also allows taking of samples of tissue for biopsies, the removal of polyps (small benign growths), and injection of bleeding blood vessels. Also useful for dilatation of strictures in the oesophagus (food pipe).
How are you prepared?
Prior to the procedure you will be asked not to eat or drink for ideally 6 hrs since your last feed. This is to allow emptying of stomach for a satisfactory examination.
How is gastroscopy done?
A soft, thin flexible tube is passed into the stomach via the mouth. This takes about 5 to 10 minutes and is done under topical anaesthesia which will be sprayed into your throat to minimise retching.
Are there alternatives to gastroscopy?
A barium meal x-ray of the stomach will give similar information but it is not as accurate in detecting ulcers and other abnormalities, and it does not allow biopsies to be taken.
Inform your doctor if you have diabetes, fits or any problem for which you are taking medicines.
Colonoscopy
What is the purpose of colonoscopy?
To examine the colon (large bowel), to remove polyps (small benign growths) to take samples of tissue (biopsies) for examination by a pathologist. Colonoscopy is the most reliable method of large bowel examination.
How are you prepared?
Prior to the day of procedure you will be given a bowel preparation kit with instructions. The bowel preparation cleans the colon. Without this it is not possible to perform a full examination of the colon. Although the bowel preparation is unpleasant, it is very rare for it to be harmful.
How is colonoscopy done?
A long, flexible tube is passed around the bowel from the anus. This takes about 15-20 minutes and is done under intravenous sedation (Midazolam and sometimes Propofol). Reactions to these medications are rare. After the procedure you must not drive or use machinery until the next day.
Are there alternatives to colonoscopy?
A barium enema x-ray of the bowel will give similar information but it is not as accurate for certain problems, it does not allow biopsies or removal of polyps. It does not require sedation or hospital admission.
Complications
Colonoscopy and polypectomy are very safe. Serious complications are rare. These include:
- Reaction or sensitivity to medication used for sedation (this may affect your breathing briefly)
- Perforation (puncture) of the lining of the bowel (about 1 patient in 2000-5000)
- Bleeding – if blood vessels are injected or a polyp is removed (about 1 patient in 300-500)
- Heart attacks, cardiac arrest, blood clots, and breathing problems (very rare)
Everything will be done to minimise the risk of these complications. There are ways of detecting these complications early and specific treatments are available if they do arise.
Special Precautions will need to be taken:
- if you suspect or know you are pregnant or if you are breastfeeding
- have severe heart, lung, or kidney disease
- have lymphoma, leukemia, or you are receiving chemotherapy
- if you have had heart valve disease, a pacemaker, aortic graft or other blood vessel graft
- if you bleed very easily or if you take blood thinning tablets (warfarin), aspirin, or arthritis tablets
- if you are allergic or sensitive to any medication
Endoscopic Retrograde Cholangio Pancreatography (ERCP)
1. How did I get stones in my bile duct?
Most often the stones from the diseased gallbladder spill or migrate into the common bile duct (CBD) and create a blockage.
2. What happens if stones in the bile duct are left untreated?
Stones in the CBD can cause severe colicky pain, fever and jaundice and sometimes life threatening pancreatitis. This is a serious condition requiring hospitalization. Should not be confused with routine infective jaundice.
3. How are the bile duct stones removed?
Stones in the bile duct require surgical removal. In the earlier times open surgery was the only option but now it is possible to have the stones removed during an ERCP.
4. What is ERCP?
ERCP is an x-ray examination which uses an endoscope to examine the bile or
pancreatic duct, which are located in relation with the small bowel. These ducts will be mapped with x-ray dye. This procedure helps to identify any abnormalities in the biliary system liver, gall bladder and pancreas.
5. What are the benefits of an ERCP?
The benefits are that it is a non-surgical procedure offering treatment, without the need for an operation.
6. How do I prepare for an ERCP?
You will be admitted to hospital on the day of the procedure. To allow a clear view with the endoscope, the stomach must be empty. You will
therefore be asked not to eat or drink for at least eight hours before your procedure.
7. What if I am on medications for my other ailments?
If you are diabetic, asthmatic or currently taking Warfarin, Clopidogrel or Aspirin please inform the doctor dealing you. You shouldn’t be taking these medicines for at least 5-7 days before procedure.
8. What happens to me in the endoscopy unit?
Before your procedure, you will be asked to give your consent. It is
important to understand that the operation/procedure is likely to involve
risks, benefits and alternatives before you sign the consent form.
9. What happens during the ERCP ?
The procedure is performed in the Endoscopy Suite with the assistance of a special type of X-Ray unit called fluoroscopy. You will be anaesthetised. After anaesthesia the endoscope will be passed through your mouth, down the food pipe into your stomach and into the small intestine (duodenum) where the entrance to the bile and pancreatic duct. Using special contrast medium( dye) the bile duct and pancreatic ducts are mapped.In about 5% of patients this is not successful. The procedure takes up to 45 minutes and you are under anaesthesia.
What is the purpose of ERCP?
To examine the bile ducts and pancreatic ducts, to remove gallstones from the bile ducts, to dilate strictures in the bile ducts, to biopsy or remove a tumour of the duodenum, pancreas or bile ducts, and to deploy a plastic or metal tube called a stent to overcome stricture.
Sphincterotomy
Sphincterntomy involves making a small cut in the lower part of the bile duct where the duct opens into the duodenum. This is done using an instrument passed through the endoscope. You do not feel the cut. This procedure allows better access into the bile duct, removal of gallstones, and other procedures to be performed.
How are the gallstones removed endoscopically?
A side viewing duodenoscope is inserted through the mouth, down the food pipe, through the stomach and into the duodenum. Once the papilla of Vater, the opening of common bile duct, is identified, a small catheter (cannula) is passed through an open channel of the endoscope into the opening of the papilla, and into the bile ducts. Contrast material (dye) is then injected and X-rays are taken of the bile ducts and the pancreatic duct. The open channel in the endoscope also allows specially designed instruments to be passed through it in order to retrieve the stones by careful trawling. The stones fall into the intestinal lumen and pass off in the stools.
Are there Alternatives to ERCP?
Sometimes ultrasound, CT cholangiography, and MRI cholangiography can give very similar information to that provided by ERCP, however these investigations do not allow therapeutic procedures to be performed. Your doctor will discuss these investigations with you if you wish.
Complications
ERCP, sphincterotomy, and stent insertion are normally safe procedures and are only done when other methods of diagnosis or treatment have failed. Complications (mostly minor) occur in about 5% of patients, including:
- Reaction or sensitivity to medication used for sedation
- Pancreatitis (inflammation of the pancreas) (mild pancreatitis occurs in about 1 patient in 20)
- Bleeding following sphincterotomy (about 1 patient in 100)
- Perforation (puncture) of the lining of the duodenum or bile duct (about 1 patient in 1000)
- Infection of the bile ducts, blood, and other organs
In experienced hands the complication rate varies from 1-5%. These complications are inherent and in built risk of this minimally invasive and technically difficult and demanding procedure. Everything will be done to minimise the risk of these complications.
The nature of the test, including possible side-effects and complications, will be discussed with you before the test. If you wish to have more information please consult your doctor before the test.
Special Precautions
Please notify your doctor:
- if you suspect or know you are pregnant (x-rays are used in this test) or if you are breastfeeding
- have severe heart, lung, or kidney disease
- if you bleed very easily or if you take blood thinning tablets (warfarin), aspirin, or arthritis tablets
24 Hr. Oesophageal pH and Impedance testing:
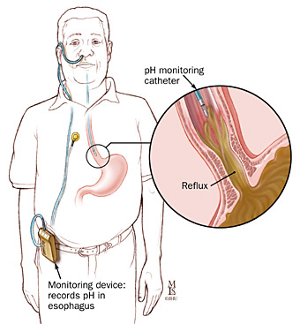 A 24-hour pH impedance test is ordered to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period.
A 24-hour pH impedance test is ordered to evaluate your reflux. This procedure monitors your pH level (level of acidity) for a prolonged period.
Why is 24-Hour pH Impedance performed?
Your oesophagus has a muscle at the entrance to the stomach in order to keep food from coming back up into the esophagus. If this valve is not working properly, you may experience heartburn, pain or coughing.
This test measures how often acid leads from your oesophagus into your stomach, and if this acid is related to your symptoms.
How is the pH impedance performed?
- A thin, flexible catheter with an acid-sensitive tip is passed through your nose into your oesophagus. The catheter is placed in separate recording spots to evaluate the flow of liquid from your stomach into your oesophagus.
- The catheter stays in your nose for a period of 24 hours.
- Your doctor is able to evaluate whether you have gastroesophageal reflux disorder (GERD)the severity of your reflux, and the correlation between your reflux and the symptoms and presence of nonacid reflux. This procedure helps your doctors design a course of treatment.
High resolution GI manometry
High Resolution Manometry (HRM) allows measuring of pressures in the gastrointestinal tract and interpretation of the results. This method consists of measuring multiple pressures simultaneously. This allows detailed assessment of all relevant data for the whole esophagus or anal sphincter.
Clinical Applications:
- High Resolution Manometry is used to measure peristalsis in the esophagus (HRM).
- HRM can also be combined with impedance measurement (HRIM) and combined with “cine loops’ to view the swallows and bolus movement in the esophagus
- To assess the functionality of apparatus and defecation provided by the anal sphincter (HRAM).
Capsule endoscopy
What is Capsule endoscopy?
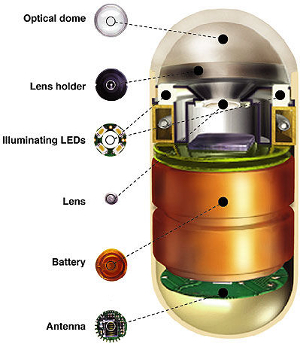 It is a procedure that uses a tiny wireless camera to take pictures of your digestive tract. A capsule endoscopy camera sits inside a vitamin-size capsule you swallow. As the capsule travels through your digestive tract, the camera takes thousands of pictures that are transmitted to a recorder you wear on a belt around your waist.
It is a procedure that uses a tiny wireless camera to take pictures of your digestive tract. A capsule endoscopy camera sits inside a vitamin-size capsule you swallow. As the capsule travels through your digestive tract, the camera takes thousands of pictures that are transmitted to a recorder you wear on a belt around your waist.
 Capsule endoscopy helps doctors see inside your small intestine — an area that isn’t easily reached with more-traditional endoscopy procedures. Traditional endoscopy involves passing a long, flexible tube equipped with a video camera down your throat or through your rectum.
Capsule endoscopy helps doctors see inside your small intestine — an area that isn’t easily reached with more-traditional endoscopy procedures. Traditional endoscopy involves passing a long, flexible tube equipped with a video camera down your throat or through your rectum.
H2 breath test
The hydrogen breath test is a test used to diagnose ‘lactose intolerance ‘ or determine if abnormal bacteria are present in the colon.
What Is Lactose Intolerance?
Lactose intolerance is the inability to digest lactose, the sugar found in milk. It causes cramping, bloating, gas, or diarrhea any time dairy products are consumed. Lactose intolerance occurs due to the body’s lack of lactase, an enzyme normally produced by the small intestine that is needed to digest lactose.
What Happens During the Hydrogen Breath Test?
During the hydrogen breath test, which takes about 2 hours, you will be asked to drink a lactose-containing beverage. The beverage may cause cramping, bloating, gas, or diarrhea.
Fifteen minutes after drinking the beverage, you will be instructed to blow up balloon-like bags every 15 minutes for two hours.
The air you breathe into these bags is tested frequently for the presence of hydrogen. Normally, very little is detected in breath. However, hydrogen and other gases are produced when undigested lactose in the colon is fermented by bacteria.
Raised hydrogen breath levels indicate the improper digestion of lactose, which could lead to a diagnosis of lactose intolerance or the presence of abnormal bacteria in the colon.
Imaging Studies
Ultra Sonogram (USG) & Endoscopic Ultrasound Study (EUS)
An ultrasound scan is a medical test that uses high-frequency sound waves to capture live images from the inside of your body.
An ultrasound allows your doctor to see problems with organs, vessels, and tissues. Unlike other imaging techniques, ultrasound uses no radiation, so it is the preferred method for viewing a developing fetus during pregnancy.
What is Endoscopic Ultrasound (EUS)?
Endoscopic Ultrasound (EUS) is a procedure that looks at your digestive system from the inside. It can be done for either your upper or lower digestive tract. An endoscope, with a tiny camera at the end, is gently guided into your digestive system. This tube also has a tiny echo machine at the end that can send out sound waves very similar to an external ultrasound. The use of sound waves allows your doctor to examine and take pictures of your digestive system and the organs and lymph nodes outside of the digestive tract. EUS produces very high resolution pictures that allow your physician to more accurately diagnose and treat your condition.
Clinical Applications:
- In addition to the diagnostic capabilities, EUS may be used to treat certain conditions of the digestive tract.
- In addition, with EUS, it is possible to inject medicine into certain areas of the GI tract.
- Biopsy: The EUS scope can also be used to direct a tiny needle into an area of concern and take a sample of tissue. This is called “Fine Needle Aspiration (FNA)”.
CT Scan:
Computerized (or computed) tomography is an X-ray procedure that combines many X-ray images with the aid of a computer to generate cross-sectional views and, if needed, three-dimensional images of the internal organs and structures of the body.
Computerized tomography is more commonly known by its abbreviated names, CT scan or CAT scan. A CT scan is used to define normal and abnormal structures in the body and/or assist in procedures by helping to accurately guide the placement of instruments or treatments.
MRI Scan
Magnetic resonance imaging (MRI) uses a large magnet and radio waves to look at organs and structures inside your body. Doctors use MRI scans to diagnose a variety of conditions, from torn ligaments to abdominal and brain tumors. MRIs are very useful not only for examining the brain and spinal cord but also liver and pancreas system.
PET scan
A positron emission tomography (PET) scan is a type of imaging test. It uses a radioactive substance called a tracer to look for disease in the body.
A PET scan shows how organs and tissues are working. This is different than magnetic resonance imaging (MRI) and computed tomography (CT), which show the structure of, and blood flow to and from organs. Many places have machines that combine the PET and CT images, so that only one exam is performed.
Why the Test is Performed?
A PET scan can reveal the size, shape, position, and some function of organs.
This test can be used to:
- Check brain function
- Diagnose cancer, heart problems, and brain disorders
- See how far cancer has spread
- Determine if a mass in your lung is cancerous or harmless
- Several PET scans may be taken over time to check how well you are responding to treatment for cancer or another illness.
Bleeding from Gastrointestinal (GI) Tract
What causes bleeding in the upper GI tract?
A variety of conditions can cause bleeding in the upper digestive tract. Locating the source of bleeding is an important step to help the doctor find the cause of the bleeding. Different conditions can cause bleeding in the upper GI tract.
Causes of bleeding in the upper GI tract may include
- Peptic ulcers—sores in the lining of the oesophagus, stomach, or duodenum. The bacteria Helicobacter pylori (H. pylori) and use of pain killers- aspirin or the nonsteroidal anti-inflammatory drugs (NSAIDs) can cause peptic ulcers.
- Oesophageal varices—enlarged blood vessels in the oesophagus (food pipe) that can leak blood or even rupture, causing life-threatening bleeding. Oesophageal varices are usually associated with a chronic liver condition called cirrhosis.
- Mallory-Weiss tear— Severe vomiting causes tears in the lower end of the oesophagus ( food pipe)
- Gastritis—a condition in which the stomach lining is inflamed. Some common causes of gastritis include the use of aspirin, NSAIDs and other medications, infections, critical illnesses, and severe injuries. If untreated, gastritis can lead to ulcers or erosions in the stomach lining that can bleed.
What are the signs and symptoms of bleeding in the digestive tract?
The signs and symptoms of bleeding in the digestive tract depend on the location and severity of bleeding.
Signs and symptoms of bleeding in the upper or lower GI tract may include
- acute bleeding, which may include abdominal cramps
- bright red blood in vomit
- dark or bright red blood mixed with stool
- vomit that looks like coffee grounds
- black or tarry stool
- dizziness or faintness
- shortness of breath
Chronic bleeding
A person with chronic bleeding may develop anaemia, a condition in which red blood cells are fewer than normal, which prevents the body’s cells from getting enough oxygen. Symptoms of anaemia may include fatigue and shortness of breath, which can develop over time.
Some people may have occult bleeding. Occult bleeding may be a sign of inflammation or a disease such as colorectal cancer. A simple lab test can detect occult blood in the stool.
A large number of endoscopic procedures are available to alleviate symptoms and can offer cure.
The therapeutic endoscopic procedure is carried out via the endoscope under anaesthesia.
The role of therapeutic endoscopy in current gastroenterology is very important. It eliminates the risk of pen surgery.
Endoscopic control of gastrointestinal bleeding includes the following procedures. Endoscopic hemostasis for bleeding ulcers eliminates the risk of surgery, is less expensive and better tolerated by patients. Owing to these procedures mortality has significantly decreased.
- Oesophageal Variceal banding
- Endoscopic glue Injection of gastric varices
- Electrocoagulation of bleeding ulcer
- Oesophageal dilatation of stricture,
- Oesophageal stenting in cancer
- Foreign body removal
- Endoscopic Sub-mucosal Mucosal Dissection
- Per Oral Endoscopic Myotomy (POEM)
Liver & Biliary System
Endoscopic Retrograde Cholangiopancreatography has a therapeutic application designed to cut the sphincter of Oddi fibers of the distal common bile duct, what is indicated currently in choledocholithiasis and papillary stenosis with ascending cholangitis, acute gallstone pancreatitis.
Endoscopic sphincterotomy in now an established procedure that is indicated in patients with common bile duct calculi.
Endoscopic decompression of the biliary tree – dilatation benign structures of the biliary tree with balloon catheters and placement of stent (internal endoprothesis) allows the non operative decompression and significant palliation for patients with obstructing tumors.
Stenting of Pancreas for pancreas divisum and stones in the pancreatic duct.
COLON
Colonoscopic polypectomy is a widely used technique. By removal of polyps the incidence of colon cancer can be decreased.
Stenting of large bowel for cancerous intestinal obstruction.